Varicose Veins
DOWNLOAD INFORMATION LEAFLET
Varicose veins are a common condition affecting up to 15 percent of men and up to 25 percent of women. The word "varicose" comes from the Latin term "varix," meaning " twisted." Any vein may become varicose, but the veins most commonly affected are those in your legs and feet. That's because standing and walking upright increases the pressure in the veins in your lower body.
What are varicose veins?
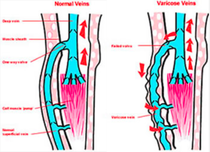
Varicose veins are "dilated tortous veins associated with incompetent venous valves" They are very common and predominately affect the legs although they can affect any part of the body. They are more pronounced when you stand up and often described by patients as being "unsightly".
Why do we get them?
In short, people with varicose veins often have a genetic tendency to developing them. This is further affected by factors such as occupation (standing for long periods) or during pregancy. All veins in the legs have valves to ensure blood travels in one direction only (upwards) each time the calf muscle squeezes. Failure of either the valves or the calf muscle pump system results in patients being susceptible to having varicose veins. The result is the development of a pressurised venous syste. This manifests itself as varicose veins over the course of time.
The main sites of valvular incompetence arise in the groin (in the groin crease) or behind the knee where the large superficial veins drain back into the larger deep veins. There can be other sites of incompetence throughout the leg but in the vast majority of individuals these 2 sites are their main problem.
Symptoms
Varicose veins are very common and in some people causes very little in the way of symptoms. However, the following are symptoms described by patients who do suffer with varicose veins:
- Aching, heavy legs usually worse at the end of the day
- Ankle swelling
- Discolouration around the veins, usually a brownish colour (Haemosiderin depaosits)
- Skin over the veins may become dry, itchy and thin, resulting in venous eczema
- The skin above the ankle may shrink because the fat underneath the skin becomes hard and scarred (Lipodermatosclerosis)
- Patients may suffer with phlebitis which is a painful inflammatory condition of the varicose veins
- Bleeding which can be quite significant (sometimes caused by a minor injury)
- Venous leg ulcers (if skin changes start occuring, such as discoloration above the ankle, itching dry skin or scarring, then there is a risk for future skin breakdown and leg ulcer development)
Treatment
A clinic assessment will establish the presence of varicose veins/ thread veins and whether they may or may not be contributing to your symptoms. Also, an assessment of the distribution of the varicose veins and the underlying "leaky" valves is necessary in order to plan treatment. This can be performed by means of a hand held doppler machine or by ultrasound technology. More often, Duplex ultrasound scans are necessary to evaluate the site of valvular incompetence and also to assess whether the veins are suitable for the less invasive techniques such as Endovenous Laser Therapy (EVLT) or Radiofrequency (eg VNUS). Tradional open surgery may be necessary and is also "tried and tested" technique which also provides excellent results.
The fundamental principle for successful treatment involves:
- Identification of the underlying valvular incompetence ("leaky valves") which are usually in the groin or behind the knee.
- Treatment of the valvular incompetence and trunk vein (eg the long thigh vein) by EVLT or traditional surgery ("Stripping of the veins" )
- Treatment of the visible varicose veins themselves by means of phlebectomy ("multiple avulsions") or sclerotherapy. Phlebectomy involves making a small (1-2mm) cut over the vein and avulsion of the varicose vein using a special hook instrument. It provides excellent results leaving a very satsifactory cosmetic appearance. Sclerotherapy involves injection of a sclerosant fluid into the varicose vein. This deliberately irritates the vein and closes it. It tends to work better with very small veins and thread veins.
Information you need to know about your operation
Before the operation
You should not eat any food for up to 6 hours before surgery but you can have a couple of glasses of water up to 2 hours before your operation.
Coming into hospital
The operation is commonly performed as a day case. However, if you have any medical problems, may require a hospital stay overnight. On admission to the ward, a nurse will take details about you and take your temperature, pulse and blood pressure. Your varicose veins will be marked whilst you stand. The operation will be explained and consent obtained by Prof M Baguneid.
Traditional surgical procedure
This will be explained in detail by Prof M Baguneid. The main feeder vein and "leaky valve" are tied off through an incision in the groin and /or behind the knee. All the pre-marked visible varicose veins are then removed (avulsed) through a series of small incisions (<2mm in length).
Endovenous laser therapy (EVLT)
This will be explained in detail by Prof M Baguneid. The faulty vein in the thigh or behind the knee is cannulated under ultrasound guidance with a needle. A catheter and laser or VNUS fibre is introduced into the veiin. The vein is then ablated from within by activating the fibre whilst it is withdrawn. All the pre-marked visible varicose veins are then removed (avulsed) through a series of small incisions (<2mm in length). The entire procedure can be performed under local anaesthetic (often with sedation). It can be performed under a general anaesthetic (asleep) if the patient is keen not to have a local anaesthetic.
After your operation
At the end of the operation you will have a bandage on your treated leg(s). A wool bandage and stocking will be underneath the outer bandage.
If you had traditional surgery, you will have dissolvable stitches in your groin wound and/or knee wound. If you had EVLT or Radiofrequency ablation, there will not be any groin or knee incisions. The avulsion sites will have adhesive paper strips. You will usually be asked to elevate your legs in bed initially but very soon afterwards you will be able to mobilise. A little discomfort is to be expected and you will be provided painkillers if required.
Going home
Stockings: You will be provided compression stockings to take home. You will need to take your bandage off the day after surgery and apply your stocking. Don't worry if any paper stitches come off at the same time. This stocking is to be kept on day and night for the first week.
Pain: Most people describe the leg as "a bit uncomfortable" when they get home but it tends to imporve over the first couple of days. There may occasionally be mild discomfort again a week after the procedure but all this usually resolves by 12-14 days after the operation. There may be tenderness, lumpiness and bruising over the inner thigh and calf for first couple of weeks. This is normal. However in the rare event that red and painful lumps appear near the operation scars you should see your GP in case there is an infection.
Exercise: Walking for fifteen minutes every hour is good, gradually building this up until you are fully mobile. You should avoid standing still or sitting with your legs down for the first week. Keep active in general in order to reduce your risk of developing a deep vein thrombosis.
Shower: It should be fine to shower after 2 days when your wounds have dried and settled. You can take your stockings off for the time you shower then reapply them once you have dried your legs gently. (Don't worry if any paper stitches come off as the tiny wounds will heal well either way). If bleeding occurs from any of the tiny wound sites, then lie down, raise the leg, and apply pressure for seven minutes over bleeding point with a towel or handkerchief. Bleeding is always easy to stop. The paper stitches should be removed after 7 days but don't be worried if any come off sooner (even 1st day following surgery).
Return to normal activities
Driving: You can drive as soon as you can apply emergency brakes without hesitation. It is likely that following endovenous treatments like EVLT or VNUS, driving should be possible the next day.
Work: You can return to work when you feel sufficiently well and comfortable. Usually this takes a week or two if you had traditional after surgery. With keyhole treatments, you should be able to return to work within the 1st week depending on your occupation and if you can return to light duties.
Sports: Swimming and cycling are usually comfortable after the adhesive strips have been removed (roughly after 7 days).
Flying: You should take advice from your airline but it is not advisable to take a long haul flight for at least 4 weeks following your operation (or EVLT). Short haul flights following "keyhole" procedures may be possible within a few days.
Benefits & Risks
Surgery or EVLT will treat varicose veins, although 5-10% patients will develop recurrence over a five-year period.
Not all leg symptoms in patients with
varicose veins are caused by these veins. Aching, itching and
swelling may be improved by surgery but not in every case.
The cosmetic result is usually very good but
the tiny incisions are often visible for first 6
months. They often fade thereafter.
Wound infections are unusual but may occur in approximately 1 in 50 patients. A small nerve to the skin may be damaged while avulsing varicose veins causing numbness for 2-3 weeks after which the absence of sensation, which is permanent, is no longer noticeable. Very rarely, persistent discomfort may persist related to nerve damage.
Deep vein thrombosis may occur following any
surgery, particularly under general anaesthetic.
Without treatment to prevent this, the risk is only 7 per 1000 operations but we will thin the blood in
patients at risk so this occurs in under 5 per 1000.